Pelvic organ prolapse
What is pelvic organ prolapse:
Pelvic relaxation is a weakness or laxity in the supporting structures of the pelvic region. Bladder, rectal, or uterine tissue may then bulge into the vagina. This is called pelvic organ prolapse.
Once rarely discussed or recognized, this problem has now become a priority in women’s health. Today, many primary care physicians and gynecologists routinely screen patients for the symptoms, and the new surgical specialty of female Urology and Urogynecology has arisen to correct prolapse conditions and the urinary incontinence that often results. By age 80, more than 1 in every 10 women will have undergone surgery for prolapse.
Types of pelvic organ prolapse
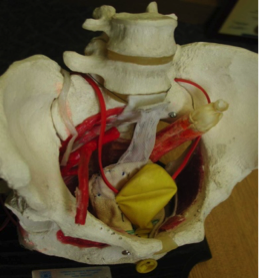
Different types of pelvic organ prolapse affect different parts of the vagina (see illustrations):
Cystocele and urethrocele.
A cystocele or urethrocele occurs when the bladder or the urethra protrudes into the front wall of the vagina. This can obstruct the flow of urine and cause difficult voiding and emptying of the bladder
Rectocele. Part of the rectum bulges into the back wall of the vagina, sometimes causing difficulty with defecation.
Uterine prolapse. The uterus drops down into the vagina. In women who have undergone a hysterectomy, a similar condition known as vaginal vault prolapse can occur: the top of the vagina protrudes into the lower vagina.
What causes pelvic organ prolapse?
Pelvic support comes from pelvic floor muscles, connecting tissue (fascia), and thickened pieces of fascia that serve as ligaments. When pelvic floor muscles are weakened, the fascia and ligaments have to bear the brunt of the weight. Eventually, they may stretch and fail, allowing pelvic organs to drop and press into the vaginal wall.
Women who have had multiple vaginal births are at greatest risk for pelvic organ prolapse, particularly after menopause. Other risk factors include surgery to the pelvic floor, connective tissue disorders, and obesity, chronic cough, smoking and constipation.
What are the symptoms?
Women with mild prolapse discovered during a routine pelvic exam may have no symptoms at all. But others experience considerable discomfort and a range of symptoms, including:
Pressure and pain. The most common complaints are a feeling of pelvic pressure, or bearing down, leg fatigue, and low back pain.
Urinary symptoms. Cystocele, urethrocele, and uterine prolapse can cause stress incontinence and difficulty in starting to urinate. In severe cases, the ureters which are the tubes that carry the urine from the kidneys to bladder can be kinked and obstructed which may damage the kidneys
Bowel symptoms. A rectocele may cause problems with defecation by forming a pocket just above the anal sphincter. Stool can become trapped, causing pain, pressure, and constipation.
Sexual problems. A prolapse can cause irritated vaginal tissues or pain during intercourse, as well as psychological stress.
If you think you have a pelvic prolapse condition, see your primary care provider or gynecologist. A traditional pelvic examination is the only way to diagnose it.
Treating prolapse
Women with no or very mild symptoms don’t need treatment, although they should avoid anything that might worsen the prolapse. Losing weight if necessary, avoiding lifting heavy objects, and quitting smoking all prevent prolapses from progressing. Prolapse doesn’t necessarily worsen over time, so there’s no need to seek aggressive treatments, unless your symptoms are really bothersome.
If you’re experiencing major discomfort or inconvenience, surgery is the only definitive way to relieve symptoms and improve your quality of life (see “Surgical treatment,” below). But if your symptoms are mild or you want to delay or avoid surgery, less invasive treatments can help:
Kegel exercises. A woman with prolapse but no symptoms may be urged to practice Kegel exercises to reduce the chance that her condition will progress. Kegel exercises are a series of contractions that strengthen the pelvic floor. You squeeze two sets of pelvic floor muscles at the same time: those you would use to prevent yourself from passing gas and those you would tighten to stop urinating. Avoid contracting your stomach muscles.
Try to do 30–40 pelvic contractions each day; you may want to divide them into three or four groups of 10 each, spread throughout the day. Squeeze and hold the contraction for 3–5 seconds; then rest for the same length of time. Build up to 10-second contractions, with 10 seconds of rest in between.
Pessary. For women who aren’t good surgical candidates or want to delay surgery (perhaps if planning to have more children), one alternative is a vaginal pessary — a device similar to a diaphragm or cervical cap that’s inserted in the vagina to help support the pelvic area (see illustration). Pessaries are kept in all the time. They should be tken out periodically to be cleaned
Surgical treatment
Before undergoing surgical repair of a prolapse, you’ll need to have a thorough pelvic exam, to ensure that all problems have been identified. Be sure your surgeon has expertise in the field of pelvic reconstruction, as new procedures and anatomical knowledge have led to better results.
Surgical techniques. Pelvic reconstruction surgery may be performed through the vagina or abdominally; both procedures are equally effective. A newer option is Robotic surgery, in which repairs are made with instruments, including a camera, inserted through a few tiny abdominal incisions. The prolapsed organ will be repositioned and secured with stitches to the surrounding tissues and ligaments. The vaginal defect will be repaired, sometimes using a piece of synthetic material, called a graft. Women can usually leave the hospital within one to three days. Recently, FDA has warned about extensive use of synthetic mesh in the vagina because of high risk of complications as erosion and infection. As a result, most cases of prolapse are now repaired using the abdominal approach. The procedure is known as abdominal colposacropexy, where the mesh is placed outside the vagina, so the risk of erosion is much less then the vaginal approach
Complications. Possible complications of pelvic reconstructive surgery include urinary tract infection, temporary or permanent incontinence, infection, bleeding, and — rarely — damage to the urinary tract that requires additional corrective surgery. Some women may develop chronic irritation or pain during intercourse from a suture or scar tissue.
There’s also a risk of recurrence, which seems to be highest for cystocele and lowest for rectocele. Fortunately, recurrence rates are dropping as surgical techniques and preoperative planning improve. The chance of recurrence will also be reduced if a woman avoids stress, such as heavy lifting or straining during a bowel movement, and performs Kegel exercises regularly before and after surgery.

Limb, J; Weinberger, M; Miyazaki, F; S R Aboseif: Sacral colpopexy using mersilene mesh in the treatment of vaginal vault prolapse. World J Urol. Feb;23 (1):55-60. 2005